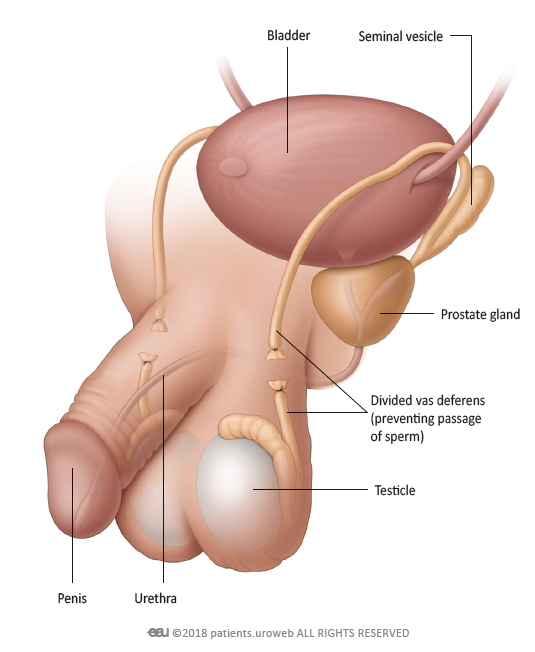
Q 1. What does the procedure involve?
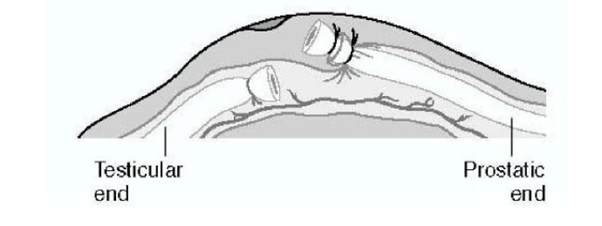
A. Removal of a small section of vas from both sides with interposition of tissue between the divided ends to prevent re-joining.
Q 2. What are the alternatives to this procedure?
A. The alternatives include other forms of contraception (both male and female).
Vasectomy should be regarded as an “irreversible” procedure. If you have any doubt about whether it is the right option for you, do not proceed with the operation.
Under normal circumstances, vasectomy will not be considered during pregnancy or within the first six months after the birth of a child.
Q 3. What should I expect before the procedure?
A. If you are taking blood thinning medication on a regular basis, you must discuss this with your urologist because these drugs can cause increased bleeding after surgery. There may be a balance of risk where stopping them will reduce the chances of bleeding but this can result in increased clotting, which may also carry a risk to your health. This will, therefore, need careful discussion with regard to risks and benefits. Aspirin does not usually need to be stopped but will be the decision of your surgeon.
You will usually be admitted on the same day as your surgery, or a day before. You will normally undergo pre assessment on the day of your clinic. After admission, you will be seen by members of the medical team which may include the consultant, junior urology doctors and nurse.
You will be asked not to eat or drink for six hours before surgery and, immediately before the operation, you may be given a pre-medication by the anaesthetist which will make you dry-mouthed and pleasantly sleepy.
Please be sure to inform your urologist in advance of your surgery if you have any of the following:
- Co-morbidities like Diabetes, Hypertension, Coronary artery disease or, stroke, epilepsy
- Any transmissible disease like HIV/AIDS, Hepatitis B or C etc
- Presence of implants, pacemakers, graft etc
- You are taking prescription drugs like-
- Blood thinners/ anti-platelets i.e. Warfarin, ecosprin, clopidogrel etc
- Anti-epileptics like phenytoin, valproate etc
Q 4. What happens during the procedure?
A. Vasectomy can be performed under local anaesthetic, a full general anaesthetic (where you will be asleep throughout the procedure) or a spinal anaesthetic (where you are awake but unable to feel anything from the waist down). All methods minimise pain; your anaesthetist will explain the pros and cons of each type of anaesthetic to you.
Q 5. What happens immediately after the procedure?
A. It is essential to have someone with you to drive you home after the procedure.
You are advised to take the following day off work and sit quietly at home. The local anaesthetic will wear off after a couple of hours and the area may ache for 24 to 72 hours; this can usually be relieved by taking Ibuprofen or Paracetamol.
Q 6. What is the duration of stay?
A. It is normally carried out on a “day care” basis with a length of stay less than one day. However, the duration of stay may extend up to 36 hours.
Q 7. What are the side effects or complications?
A. Most procedures have a potential for side effects. You should be reassured that, although all these complications are well recognised, the majority of patients do not suffer any problems after a urological procedure.
Common (greater than one in 10)
- A small amount of bruising and scrotal swelling is inevitable for several days
- Seepage of a small amount of yellowish fluid from the incision several days later
- Blood in the semen for the first few ejaculations
- The procedure should be regarded as irreversible. Although vasectomy may be reversed, this is not always effective in restoring fertility, especially if more than seven years have lapsed since the vasectomy
- Sufficient specimens of semen must be produced after the operation until they have been shown to contain no motile sperms on two consecutive specimens
- Contraception must be continued until no motile sperms are present in two consecutive semen samples
- Chronic testicular pain (10-30%) or sperm granuloma (tender nodule at the site of surgery)
Occasional (between one in 10 and one in 50)
- Significant bleeding or bruising requiring further surgery
- Inflammation or infection of the testes or epididymis requiring antibiotic treatment
Rare (less than one in 50)
- Early failure of the procedure to produce sterility (one in 250 to 500)
- Re-joining of vas ends, after negative sperm counts, resulting in fertility and pregnancy at a later stage (one in 4000)
- No evidence that vasectomy causes any long term health risks (eg testicular cancer, prostate cancer)
Q 8. What should I expect when I get home?
A. Over the first few days, the scrotum and groins invariably become a little uncomfortable and bruised. It is not unusual, after a few days, for the wound to appear swollen and slightly weepy. If you are at all worried about this, you should contact your urologist.
Q 9. What else should I look out for?
A. If you develop a temperature, increased redness, throbbing or drainage at the site of the operation, please contact your urologist.
Q 10. What are other important points?
A. You are not sterile immediately after the operation because some sperms have already passed beyond the site where the tubes are tied off.
These sperms are cleared by normal ejaculation; it takes, on average, 20 to 30 ejaculations before you are likely to be clear.
At 16 and 20 weeks after the operation you will be asked to produce specimens of semen for examination under a microscope; please read the instructions for production and delivery of these specimens very carefully. If no sperms are present, you are sterile.
If there are still a few non-motile or dead sperms, you may be regarded as sterile but, if there are large numbers of motile sperms, further specimens will be required until you are clear.
Until you get the “all clear” you must continue with your contraceptive precautions.
