Q 1. What is assisted vaginal birth?
A. An assisted vaginal birth is when a obstetrician uses specially designed instruments to help you give birth to your baby (also known as operative vaginal birth).
Q 2. Why might I need help with the birth of my baby?
A. There can be many reasons for needing help with the birth of your baby. The main ones are:
- There are concerns about your baby’s wellbeing during birth
- Your labour is not progressing as would usually be expected
- You are unable to, or have been advised not to, push during birth.
Q 3. How common is an assisted vaginal birth?
A. Overall about 1 in 8 (10-15%) births may be an assisted vaginal birth although this is much less common in women who have had a vaginal birth before.
1 in 3 women having their first baby may have an assisted vaginal birth.
Q 4. Can I avoid an assisted vaginal birth?
A. If you have someone supporting you throughout your labour you are less likely to need an assisted vaginal birth, particularly if the support comes from someone you know, in addition to your obstetrician.
Assisted vaginal births are less likely if you do not have any complications in your pregnancy.
Using upright positions or lying on your side after your cervix is fully open in labour can reduce the need for an assisted vaginal birth.
Having an epidural for pain relief in labour may increase the chance of you needing an assisted vaginal birth, but this is less likely with modern epidural anaesthetics.
The need for an assisted vaginal birth may be reduced by not starting to push too soon after your cervix is fully open. You may be advised to wait until you have a strong urge to push, or to try and delay pushing by 1-2 hours depending on your individual situation.
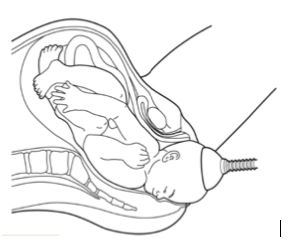
Q 5. What is a ventouse birth?
A. A ventouse (vacuum cup) is an instrument that uses suction to attach a plastic or metal cup on to your baby’s head.
Your obstetrician will wait until you are having a contraction and then ask you to push while they pull to help you give birth. This may happen over several contractions.
Sometimes the cup can detach making a ‘pop’ sound. If this happens your obstetrician may need to re-apply the cup to your baby’s head before continuing.
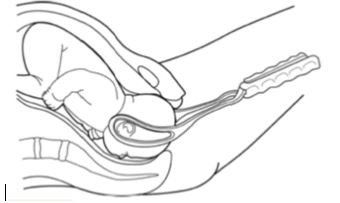
Q 6. What is a forceps birth?
A. Forceps are smooth, curved metal instruments. They are made to carefully fit around your baby’s head.
Your obstetrician will wait until you have a contraction and then ask you to push while they pull with the forceps to help you give birth. This may happen over several contractions.
Q 7. Do I have a choice between ventouse and forceps?
A. Ventouse and forceps are both safe and effective. Choice of instrument depends on factors including:
- How well your epidural is working (if you have had one)
- The wellbeing of your baby and
- The position of your baby’s head
If you need an assisted vaginal birth at less than 36 weeks of pregnancy, forceps may be preferred over ventouse.
This is because they involve less risk of injury to your baby’s head which is softer at this stage of pregnancy.
If one instrument has been chosen and is not effective, your obstetrician may then either recommend using the other instrument to help you have a vaginal birth or offer a caesarean, depending on your individual circumstances.
If neither instrument is effective in helping you give birth, your obstetrician will recommend an emergency caesarean birth.
Q 8. What are my alternatives to assisted vaginal birth?
A. Forceps and ventouse will only be recommended if they are thought to be the safest way to help you give birth.
The reasons for recommending an assisted vaginal birth, the choice of instrument and the procedure will be discussed with you at the time.
If you are in labour and choose not to have an assisted vaginal birth, the alternatives are:
- To wait for your baby to be born without assistance or
- To have an emergency caesarean.
Your obstetrician will discuss your options depending on your individual circumstances.
A caesarean in the late stage of labour is a more complex operation than a planned caesarean and, in some circumstances, may increase the risk of harm to both you and your baby.
Decision making in labour can be difficult which is why it is important to explore any concerns you may have with your obstetrician before you go into labour.
If you are certain you would not want an assisted vaginal birth, one option is to choose a planned caesarean birth before you go into labour.
Q 9. What happens during a forceps or ventouse assisted vaginal birth?
A. With your consent, your obstetrician will examine your abdomen and perform an internal examination to confirm that an assisted vaginal birth is safe for you and your baby.
You will usually be asked to sit with your legs supported and your bladder will be emptied by passing a small tube (catheter) into it.
Pain relief for the birth may be either a local anaesthetic injection inside the vagina or a regional anaesthetic injection into your back (an epidural or a spinal).
You are more likely to need to have a cut (episiotomy) to enlarge your vaginal opening and allow your baby to be born.
A neonatologist who specialises in the care of newborn babies may be there when you give birth in case your baby needs some extra help after birth.
If your baby is well you may choose to have immediate skin to skin contact and/or delayed cord clamping.
After your baby is born you will be given some antibiotics through a drip to reduce the chance of you developing an infection.
Q 10. Where will my baby be born?
A. If your obstetrician expect your assisted vaginal birth to be straightforward, they will recommend that you give birth in the same room where you have been in labour.
If they think that the assisted vaginal birth may be more complicated or that there is a chance that it might not work, you will be advised to give birth in the operating theatre. This is so that you can have an immediate caesarean if necessary.
Q 11. What makes an assisted vaginal birth less likely to be successful?
A. Assisted vaginal birth is less likely to be successful if:
- You are overweight with a body mass index (BMI) over 30
- You are less than 161cm in height
- Your baby is estimated to be more than 4kg in weight
- Your baby is lying with its back to your back at the end of your labour
- Your baby’s head is not low down in the birth canal at the end of your labour.
Q 12. What will an assisted vaginal birth mean for me?
A. You may need to stay in hospital for longer than originally expected after the birth of your baby.
Bleeding
It is normal to have vaginal bleeding after you have given birth. Straight after an assisted vaginal birth, heavier bleeding is more common. The bleeding in the days afterwards should be similar to an unassisted vaginal birth.
Vaginal tears/ episiotomy
Birth with ventouse and with forceps does mean a higher chance of needing to have an episiotomy or having a vaginal tear.
If you have either a vaginal tear or an episiotomy, this will be repaired straight after birth with dissolvable stitches.
A third- or fourth-degree tear (a tear which involves the muscle and/or the wall of the anus or rectum) affects 3 in 100 women (3%) who have a vaginal birth. It is more common following a ventouse birth, affecting up to 4 in 100 women (4%) and following a forceps birth, affecting between 8 and 12 women in every 100 (8–12%).
Pain relief
Most women have some discomfort or pain after they have given birth. You will be offered regular pain relief after an assisted vaginal birth.
Bladder care
If you have had an assisted vaginal birth you are more likely to have difficulty passing urine after birth. If you have had an epidural, you may not be able to feel your bladder getting full and may need a catheter to help empty your bladder for a few hours until your epidural wears off.
It is important that you empty your bladder completely after birth to reduce the risk of longer term problems with passing urine. Your obstetrician may ask you to pass urine in a jug so they can measure the amount. If they think that you haven’t been able to fully empty your bladder, they may use either an ultrasound or a catheter to check.
Leaking urine is common in late pregnancy and after birth. Physiotherapy may help to treat symptoms of urinary incontinence. If you have any concerns, you should discuss these with your obstetrician who can refer you to further support.
Reducing the risk of blood clots
Being pregnant increases the risk of blood clots in your legs and lungs. This risk increases after an assisted vaginal birth.
You can help to reduce the chance of this happening by being as mobile as you can after your baby is born.
Depending on your individual circumstances you may be offered blood thinning injections to reduce the risk of you developing clots.
Q 13. What will an assisted vaginal birth mean for my baby?
A. Most babies born by assisted vaginal birth are well and do not have any long term problems.
The suction cup used for a ventouse birth often causes a mark on a baby’s head. This is called a chignon (pronounced sheen-yon) and usually disappears within 24–48 hours.
The suction cup may also cause a bruise on a baby’s head called a cephalo haematoma. This happens in between 1 to 12 in 100 babies and it disappears with time. It rarely causes any problems for babies.
Forceps marks on the baby’s face are very common. They are usually small and disappear within 24–48 hours. Small cuts on the baby’s face or scalp are also common (occurring in 1 in 10 assisted vaginal births) and heal quickly.
Less common risks include:
- Jaundice, 5 to 15 in 100 babies
- Bleeding in baby’s brain, 5 to 15 in 10 000 babies
Serious trauma such as fractures or damage to nerves in the baby’s face are rare.
Q 14. How will I feel after I leave hospital?
A. Most women recover well after their assisted vaginal birth. After any birth, including an assisted vaginal birth, you may have some pain. The stitches and swelling may make it painful when you go to the toilet to pass urine or stool.
Regular pain relief will help.
You can begin to have sex again when you feel that it’s the right time for you.
Q 15. Will I need an assisted vaginal birth next time?
A. Having an assisted vaginal birth does not mean you will need one in your next pregnancy.
Most women (up to 9 in 10) who have an assisted vaginal birth have a vaginal birth next time round without needing assistance.
Q 16. What are the Key points?
A.
- Approximately 1 in 8 women have an assisted vaginal birth and this is more likely (1 in 3) for women having their first baby.
- Assisted vaginal birth includes birth helped by use of a ventouse (vacuum cup) or forceps or both. Your obstetrician will discuss the benefits and risks of assisted vaginal birth with you.
- The majority of babies born this way are well at birth and do not have any long term problems.
- Having an assisted vaginal birth does not mean you will need one in your next pregnancy.
