Q 1. What is endometriosis?
A. Endometriosis is a condition where tissue similar to the inner lining of the womb (endometrium) is found elsewhere, usually in the pelvis around the womb, ovaries and fallopian tubes.
It is a very common condition, affecting around 1 in 10 women.
You are more likely to develop endometriosis if your mother or sister has had it.
Endometriosis usually affects women during their reproductive years. It can be a long-term condition that can have a significant impact on your general physical health, emotional wellbeing and daily routine.
Q 2. What are the symptoms?
A. Common symptoms include:
- Pelvic pain
- Painful, sometimes irregular or heavy periods
- Pain during or after sex
- Fertility problems
- Pain related to your bowels, bladder, lower back or the tops of your legs
- Long-term fatigue.
Some women with endometriosis do not have any symptoms.
Endometriosis can cause pain that occurs in a regular pattern, becoming worse before and during your period.
Some women experience pain all the time but for others it may come and go.
The pain may get better during pregnancy and sometimes it may disappear without any treatment.
Q 3. What causes endometriosis?
A. The exact cause of endometriosis is not known but it is hormone dependent. This means that, just like the endometrium which responds to hormonal changes resulting in a period, the endometrial-like tissue located outside the womb also bleeds. This bleeding can cause pain, inflammation and scarring, and can possibly damage your pelvic organs.
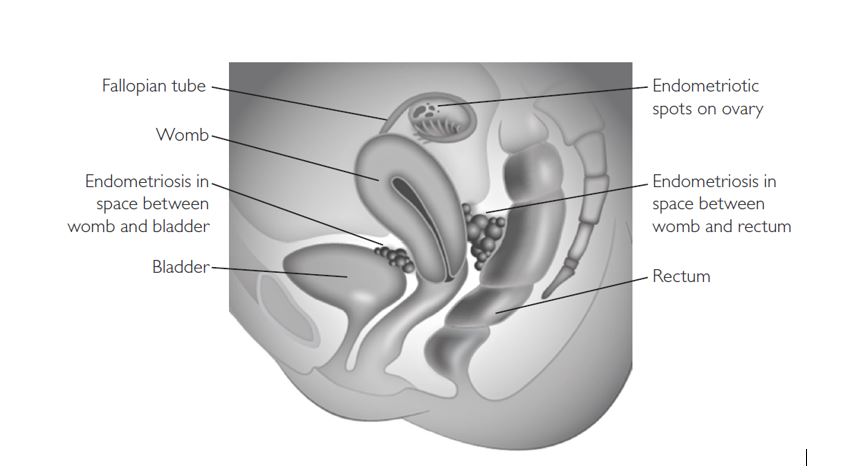
Endometriosis may be found:
- On the ovaries, where it can form cysts (often referred to as endometriomas or ‘chocolate cysts’)
- In the peritoneum (the lining of the pelvis and abdomen)
- In or on the fallopian tubes
- On, behind or around the womb
- In the area between the vagina and the rectum.
Endometriosis can also occur within the muscle wall of the womb (adenomyosis) and occasionally on the bowel and/or bladder. It may sometimes be found in other parts of the body, but this is rare.
Q 4. How is it diagnosed?
A. Endometriosis can be a difficult condition to diagnose.
This is because:
- The symptoms of endometriosis vary so much
- The symptoms are common and can be similar to pain caused by other conditions such as irritable bowel syndrome (IBS) or pelvic inflammatory disease (PID)
- Different women have different symptoms
- Some women have no symptoms.
Q 5. What will happen if I see a healthcare professional?
A. You would be asked:
- About any pain you have and whether it has a pattern or is related to anything, in particular your periods
- About your periods – are they painful and how heavy are they?
- Whether you have any pain or discomfort during sex
- About problems with your bowels or urinary symptoms at the time of your period
- About any difficulty you may have experienced getting pregnant if you have one or more of the above symptoms.
Your doctor may carry out an internal examination with your consent. This helps to localise the pelvic pain and the doctor can feel for any lumps or tender areas.
You will be able to discuss any concerns and you will have an opportunity to ask other questions.
Your doctor may offer further tests, for example an ultrasound scan, and start treatment to help your symptoms.
Q 6. What tests might I be offered?
A. Tests usually include a pelvic ultrasound scan. This may be a transvaginal scan to check the uterus and ovaries. It may show whether there is an endometriotic (also known as a ‘chocolate’) cyst in the ovaries or may suggest endometriosis between the vagina and rectum.
You may be offered a laparoscopy, which is the only way to get a definite diagnosis. This is carried out under a general anaesthetic. Small cuts are made in your abdomen and a telescope is inserted to look at your pelvis. You may have a biopsy to confirm the diagnosis and images may be taken for your medical records.
Your docotr may suggest treating the endometriosis at the time of your first laparoscopy, either by removing cysts on the ovaries or treating any areas on the lining of your pelvis. This may avoid a second operation. Sometimes, however, the extent of endometriosis found means that you may need further tests or treatment.
The procedure, including any risks and the benefits, will be discussed with you. After your operation you be will told the results.
MRI scan may be suggested if the condition appears to be advanced.
Q 7. What are my options for treatment?
A. The options for treatment include those listed below.
- Pain-relieving medication
- Hormone treatments
- Surgery
- Fertility treatment
- Other options/ complementary therapy
Q 8. What are the available medical treatment?
A. the available medical treatments include:
Pain-relieving medication
There are several different medications to help relieve your pain. These can range from over-the-counter remedies to prescribed medications from your healthcare professional. In more severe situations, you may be referred to a specialist pain management team.
Hormone treatments
These treatments reduce or stop ovulation (the release of an egg from the ovary) and therefore allow the endometriosis to shrink by decreasing hormonal stimulation.
Some hormone treatments that may be offered are contraceptive and will also stop you becoming pregnant. They include:
- The combined oral contraceptive (COC) pill or patch given continuously without the normal pill-free break; this usually stops ovulation and temporarily either stops your periods or makes your periods lighter and less painful
- An intrauterine system (IUS/Mirena®), which helps to reduce the pain and makes periods lighter; some women using an IUS get no periods at all
- Progestogens in the form of injection, the mini pill or the contraceptive implant.
Other hormonal treatments are available but these are not contraceptives. Therefore, if you do not want to become pregnant, you will need to use a contraceptive as well. Non-contraceptive hormone treatments include:
- Progestogens in the form of tablets
- GnRHa (gonadotrophin-releasing hormone agonists), which are given as injections, implants or a nasal spray. They are very effective but can cause menopausal symptoms such as hot flushes and are also known to reduce bone density. To help reduce these side-effects and bone loss, you may be offered ‘add-back’ therapy in the form of hormone replacement therapy (HRT).
Q 9. What is the available surgical treatment?
A. Surgery can treat or remove areas of endometriosis. The surgery recommended will depend on where the endometriosis is and how extensive it is. This may be done when the diagnosis is made or may be offered later. Success rates vary and you may need further surgery. Your gynaecologist will discuss the options with you fully.
Possible operations include:
- Laparoscopic surgery – when patches of endometriosis are destroyed or removed
- Laparotomy – for more severe cases. This is a major operation that requires a cut in the abdomen so that areas affected with endometriosis can be removed to provide symptom relief. This may involve removing large endometriotic cysts from your ovaries or even removal of your ovaries with or without performing a hysterectomy (removing the womb).
You will not be able to have children after a hysterectomy.
Longer term pain relief is more likely if your ovaries are removed.
However, because of the health risks associated with removal of ovaries, your doctor will discuss this and the possible need for hormone replacement therapy (HRT) with you.
Sometimes other surgeons, such as bowel specialists, will be involved in your surgery. If you have severe endometriosis, you will be referred to an endometriosis specialist centre where a specialist team that could include a gynaecologist, a bowel surgeon, a radiologist and specialists in pain management will discuss your treatment options with you.
Q 10. What are the other options or complementary treatment available?
A. Some women have found the following measures helpful:
- Exercise, which may improve your wellbeing and may help to improve some symptoms of endometriosis
- Cutting out certain foods such as dairy or wheat products from the diet
- Psychological therapies and counselling.
Complementary therapies
Although there is only limited evidence for their effectiveness, some women may find the following therapies help to reduce pain and improve their quality of life:
- Reflexology
- Transcutaneous electrical nerve stimulation (TENS)
- Acupuncture
- Vitamin B1 and magnesium supplements
- Traditional Chinese medicine
- Herbal treatments
- Homeopathy
Q 11. How will it affect my fertility?
A. Getting pregnant can be a problem for some women with endometriosis.
Hormonal treatment is not advisable when you are trying to conceive and surgical treatment may be more appropriate.
Your doctor should provide you with information about your options and arrange timely referral to a fertility specialist if appropriate.
Q 12. What are the key points to remember?
A. The key points to remember are:
- Endometriosis occurs when tissue similar to the inner lining of the womb (endometrium) is found elsewhere, usually in the pelvis around the womb, ovaries and fallopian tubes.
- Endometriosis can sometimes be a difficult condition to diagnose. It is a chronic condition that can affect your physical, sexual, psychological and social wellbeing.
- Common symptoms include pelvic pain and painful, sometimes irregular or heavy periods.
- It can cause pain during or after sex and can lead to fertility problems.
- Treatment options include pain-relieving medications, hormones and/or surgery.
