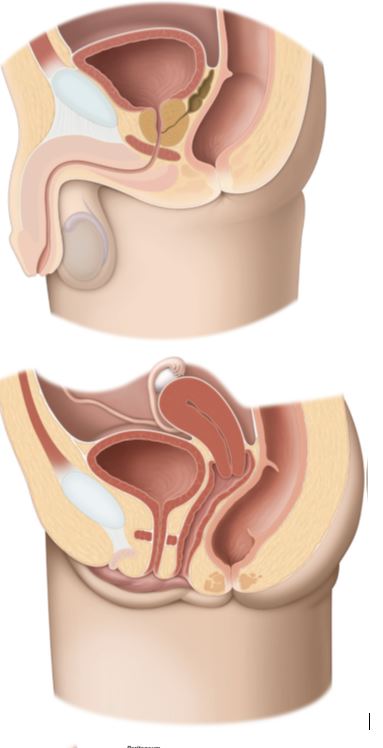
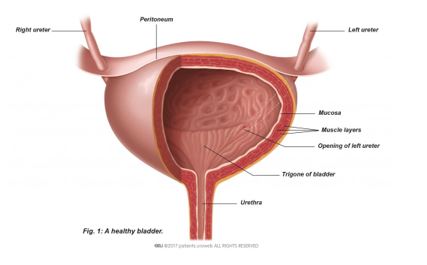
Q1. What is Urinary bladder?
A. The urinary bladder is the organ that collects and stores urine produced by the kidneys. It is a hollow and stretchable organ made of muscle tissue that sits on the pelvic floor muscles. The bladder expands as urine from the kidneys collects before being passed out of the body through the urethra.
Q 2. What is bladder cancer?
A. Bladder cancer is the growth of abnormal tissue (tumour) in the bladder. There are several stages of bladder cancer. Your treatment and experience will depend on the specific characteristics i.e staging of the tumour.
Q 3. What causes bladder cancer? What are the risk factors for this disease?
A. Several biological factors and harmful substances can increase the risk of developing bladder cancer. It develops slowly and is more common in older people (age 60 and older). According to the European Association of Urology’s bladder cancer guidelines, tobacco smoking contains many harmful substances and is responsible for almost half of the bladder cancer cases.
Another well-known source of risk is occupational exposure to chemicals used in the production of paint, dye, metal and petroleum.
Infections from certain parasites and chronic urinary tract infections increase risk of developing bladder cancer.
Sometimes bladder cancer develops without any known cause.
Q 4. What are the stages of the disease?
A. A tumour that grows towards the centre cavity of the bladder without growing into the muscle tissue of the bladder is called non–muscle invasive. These tumours are superficial and represent an early stage. This is the most common type of bladder cancer. In most cases, these tumours are not aggressive and rarely spread to other organs, so they are not usually lethal, they can however appear again (=recurrence) or develop aggressive features (=progression).
As the cancer grows into the muscle of the bladder and spreads into the surrounding muscles, it becomes muscle-invasive bladder cancer. This type of cancer has a higherchance of spreading to other parts of the body (metastatic disease) and is harder to treat. In some cases, it may be fatal.
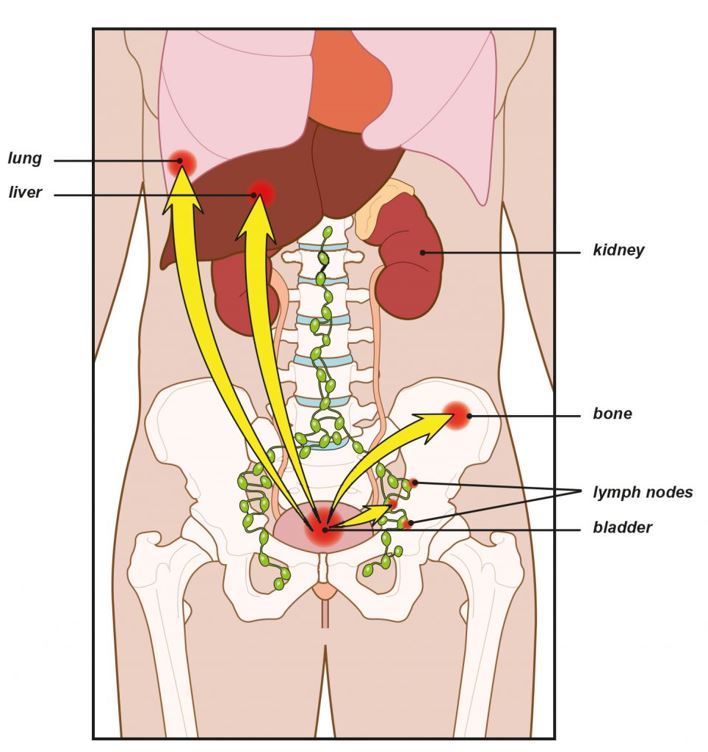
If bladder cancer spreads to other parts of the body such as the lymph nodes or other organs, it is called locally advanced or metastatic bladder cancer. At this stage, cure is unlikely, and treatment is limited to controlling the spread of the disease and reducing the symptoms.
Q 5. How can bladder cancer be prevented?
A. It is important to maintain a healthy lifestyle. If you smoke, try to stop.
Follow workplace safety rules and avoid exposure to harmful chemicals.
Some evidence suggests that drinking a lot of fluids, mainly water, might lower bladder cancer risk.
Eating a balanced diet with lots of fruits and vegetables has health benefits and might protect against cancer.
Q 6. What are the signs and symptoms of bladder cancer?
A. Blood in the urine(= hematuria) is the most common symptom when a bladder tumour is present. Tumours in the bladder lining (non–muscle-invasive) do not cause bladder pain and usually do not present with lower urinary tract symptoms (urge to urinate, irritation).
If you have urinary tract symptoms such as painful urination or need to urinate more often, a malignant tumour might be suspected, particularly if an infection is ruled out or treated and this does not reduce the symptoms. Muscle-invasive bladder cancer can cause symptoms as it grows into the muscle of the bladder and spreads into the surrounding muscles.
Symptoms like pelvic pain, pain in the flank, weight loss, or the feeling of a mass in the lower abdomen may be present in some cases when tumours are more advanced.
Q 7. How is bladder cancer diagnosed?
A. Diagnosis of cancer bladder involves history taking, clinical examination including Digital Rectal Examination (DRE), Urine examination, Ultrasonography, Cystoscopy, CT Scan or MRI scan.
Q 8. What are the different modalities employed for diagnosis of cancer bladder?
A. Urine Tests: Urine examination is performed to look for cancer cells and to exclude other possibilities like urinary tract infections. This may be referred to as ‘urinary cytology’.
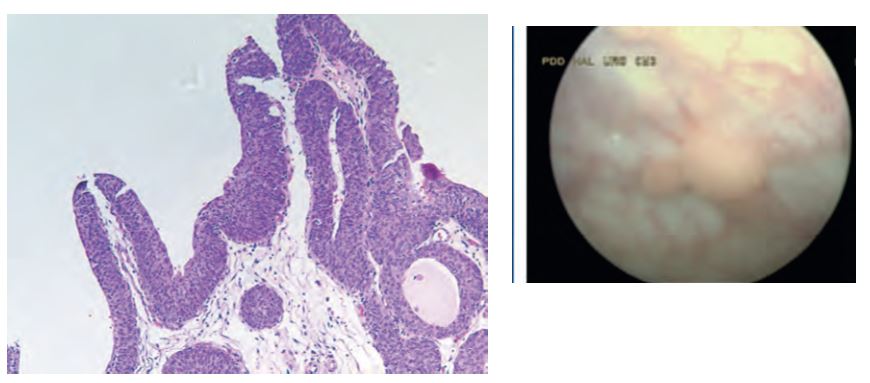
Cystoscopy: Cystoscopy is the main test used to diagnose bladder cancer. It allows your doctor to look at the inside of your bladder and urethra using a thin, lighted tube called a cystoscope.
CT urography: Computed tomography (CT scan) urography gives your doctor information about possible tumours in the kidneys or ureters and information about the lymph nodes and abdominal organs. CT urography (underline CT-urography) cannot detect small or superficial tumours (CIS). If small or superficial tumours are suspected further tests are needed.
MRI: Like CT scans, MRI scans show detailed images of soft tissues in the body. But MRI scans use radio waves and strong magnets instead of x-rays.
Transabdominal ultrasound: Ultrasound is a non-invasive diagnostic tool that can visualise masses larger than 5-10mm in a full bladder. It cannot detect very small or superficial tumours (CIS).
Transurethral resection of bladder tumor (TURBT): TURBT is the surgical removal (resection) of bladder tumour. It is both diagnostic and therapeutic.
It is diagnostic because the surgeon removes the tumour and all additional tissue necessary for examination under a microscope (histological assessment).
TURBT is also therapeutic because complete removal of all visible tumours is the treatment for this cancer. Complete and correct TURBT is essential for good prognosis.
In some cases, a second TURBT is required after several weeks.
Q 9. How do you classify bladder tumor?
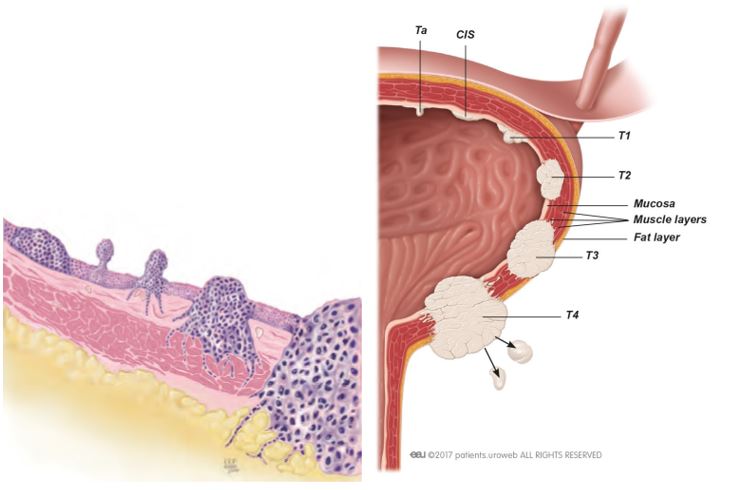
A. Bladder tumours are classified by tumour stage and subtype and by grade of aggressiveness of the tumour cells. Staging is a standard way to describe the extent of cancer spread.
1) Non–muscle-invasive bladder cancer:
Non–muscle-invasive bladder cancer, also called superficial bladder cancer, is a superficial cancer that has not grown into deeper layers of the bladder wall.
There are three subtypes based on how they grow:
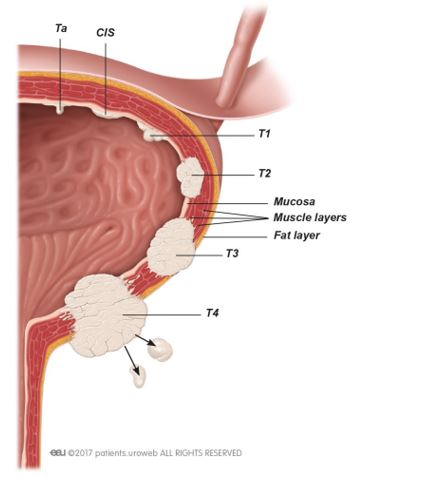
- Stage Ta tumours are confined to the bladder lining.
- Stage T1 tumours have invaded the connective tissue under the bladder lining but have not grown into the muscle of the bladder wall.
- Stage Tis tumours are flat velvet-like tumours, also known as carcinoma in situ (CIS), that are confined to the bladder wall but have potentially a high risk of spreading into the deeper layers of the bladder.
Stage Ta and T1 tumours usually appear as small grapelike growths (also called papillary) that grow toward the centre of the bladder without growing into the deeper bladder layers.
2) Muscle-invasive bladder cancer
About a quarter of patients diagnosed with bladder cancer have a muscle-invasive form that has grown into the muscular part of the bladder wall (stages T2–T4).
This type of cancer has a higher chance of spreading to other parts of the body (metastatic) and needs a different and more radical form of treatment. Muscle-invasive bladder cancer will be fatal if untreated.
Computed tomography (CT scan) is particularly important for further work-up in muscle-invasive bladder cancer. With a whole-body CT scan, done in less than 10 minutes, the physician can tell if the cancer has already grown out of the bladder and into the surrounding at tissue or adjacent organs and if there are signs of spreading to other organs (metastatic disease). By adding intravenous contrast agent, which is excreted into the urine by the kidneys, the urinary tract above the bladder can be visualised and tumour growth identified.
Prior to treatment, it is essential to evaluate whether the cancer is metastatic. If the CT scan indicates that the cancer has spread to your soft (visceral) organs, your bones or lymph nodes. This will possibly change the treatment decisions.
Additional magnetic resonance imaging (MRI scans) or bone scans may be performed, although this is not routinely done. Bone and brain metastases are rare at the time that muscle invasive bladder cancer is diagnosed. Unclear findings might also be probed with a needle biopsy to confirm metastatic disease.
A combination of positron emission tomography (PET scan; uses a radioactive tracer) and CT scan (PET/CT) is increasingly being used in European centres, although it is not generally available in all countries. PET/CT may improve the ability to detect distant metastases. It is not recommended for staging bladder tumours because urinary excretion of the radioactive tracer makes tumour staging very difficult.
Prognosis and risk stratification
The long-term prognosis for patients with muscle-invasive bladder cancer is determined by the extent of tumour growth (stage). As opposed to non-muscle-invasive bladder cancer, aggressiveness (grade) which is determined by the pathologist is less important, since virtually all invasive tumours are high grade.
3) Metastatic disease
If your bladder cancer has spread to another body organ, treatment is unlikely to cure you. Treatment options are limited to controlling the spread of disease (metastasis) and reducing symptoms.
Q 10. What are the available treatment options?
A. Following treatments are available for bladder cancer:
Transurethral resection of bladder tumor (TURBT): TURBT is the surgical removal (resection) of bladder tumour. It is both diagnostic and therapeutic.
It is diagnostic because the surgeon removes the tumour and all additional tissue necessary for examination under a microscope (histological assessment).
TURBT is also therapeutic because complete removal of all visible tumours is the treatment for this cancer. Complete and correct TURBT is essential for good prognosis.
In some cases, a second TURBT is required after several weeks.
Instillation treatment: TURBT can eradicate stage Ta or T1 tumours, but some tumours commonly recur and can progress to invasive cancer. Intravesical (within the bladder) instillation treatment after TURBT should be considered for all patients.
Removal of the urinary bladder (cystectomy): The mainstay of treatment for muscle-invasive bladder cancer is surgical removal of the urinary bladder. The indications are as follows:
- Presence of a muscle-invasive tumour
- Presence of a tumour that grows aggressively (high grade), that has multiple cancerous areas (multifocal), or that is superficial, but has recurred after chemotherapy or immunotherapy
- Failure of or recurrence after a bladder-sparing approach (chemoradiation) or the occurrence of major side-effects
- Symptoms like bleeding or pain in patients with incurable disease
Factors like your biological age (your body’s performance as it ages, measured as performance status or life expectancy) and other diseases that you have (diabetes, heart disease, high blood pressure) are also important. Patients older than 80 years of age have more problems recovering from such an operation. Being overweight does not influence survival after surgery but does influence the risk of complications from wound healing.
Removal of the urinary bladder includes removal of the bladder, the endings of the ureters and the pelvic lymph nodes. Depending on factors like tumour location and type of urinary diversion part of the adjacent gender-specific organs (the prostate and seminal vesicles in men; the entire urethra, adjacent vagina, and uterus in women) are removed. Men should be aware that prostate cancer is sometimes found in removed prostates but generally does not affect long-term survival or treatment.
If your bladder is removed, another way to store and empty urine must be created. This is known as a urinary diversion.
Bladder-sparing treatments: A bladder-sparing approach is currently used in a minority of cases worldwide but deserves consideration. Bladder preservation can be achieved at the cost of multiple therapies, including their side-effects.
Transurethral resection of the bladder tumour (TURBT) and radiation is used to cure or control the tumour locally. Chemotherapy is used to treat the cancer cells that might already have spread within in the body (systemic disease). The goal is to preserve the bladder and its function as well as quality of life without compromising cancer treatment.
About a third of patients still undergo bladder removal after failure of a bladder-sparing treatment.
Q 11. What bladder sparing treatments are available?
A. A bladder-sparing approach is currently used in a minority of cases worldwide but deserves consideration. Bladder preservation can be achieved at the cost of multiple therapies, including their side-effects.
Transurethral resection of the bladder tumour (TURBT) and radiation is used to cure or control the tumour locally. Chemotherapy is used to treat the cancer cells that might already have spread within in the body (systemic disease). The goal is to preserve the bladder and its function as well as quality of life without compromising cancer treatment.
About a third of patients still undergo bladder removal after failure of a bladder-sparing treatment.
Transurethral resection of bladder tumour: If you cannot undergo extended surgery, TURBT is possible if the tumour invades only the inner muscle layer of the bladder. With high recurrence and progression rates, this treatment alone cannot be considered a good option for controlling the disease long term.
Chemoradiation: Radiation therapy combined with sensitizing chemotherapy is a reasonable alternative for patients who refuse or are not candidates for bladder removal. Evaluation for this approach will consider general fitness (life expectancy), kidney function, prior radiation, prior abdominal operations, and history of other cancers. A consultation with a radiation oncologist is advisable prior to deciding on this treatment.
Radiotherapy: Radiation therapy is an option for preserving the bladder in patients who are not candidates for surgery or who do not want surgery. Results from radiotherapy alone are worse than those from complete removal of the bladder, but if combined with chemotherapy (chemoradiation), acceptable results can be achieved. Side-effects include mild to strong irritation of the bladder and digestive tract as well as incontinence, increased risk of infections, and fistulae (abnormal passages that develop between organs).
Chemotherapy: Chemotherapy alone has only limited results and is not recommended as a sole treatment.
Q 12. What are the treatment options for metastatic disease?
A. If your bladder cancer has spread to another body organ, treatment is unlikely to cure you. Treatment options are limited to controlling the spread of disease (metastasis) and reducing symptoms.
Chemotherapy: In 90-95% of bladder cancer cases the histological type is urothelial carcinoma. Chemotherapy that contains platinum is the most effective treatment against this type of cancer.
Chemotherapy combinations like MVAC (which uses the drugs methotrexate, vinblastine, Adriamycin [doxorubicin], and cisplatin) or gemcitabine and cisplatin are prescribed most often. These treatments have side-effects that must be considered carefully if you cannot recover from your illness.The goal is to optimise your quality of life. Limited ability to perform daily activities (low performance status), other illnesses, or decreased kidney function could make you ineligible for these chemotherapies.
If you have reduced kidney function and cannot take the drug cisplatin, combinations like gemcitabine and carboplatin or M-CAVI (which uses the drugs methotrexate, carboplatin, and vinblastine) are slightly less effective options for treating bladder cancer.
Should your disease recur or progress while taking these therapies, treatment can be changed to another type of chemotherapy, but since there is no standard in this case, the choice will depend on you treating physician.
Additional surgery to remove a metastatic or recurrent tumour mass is used only to relieve pain or obstruction and will not cure the disease.
Radiotherapy can also be used to treat symptoms like pain or recurrent bleeding (haematuria).
Some types of chemotherapy are quite intensive and can have a lot of side-effects. If you are not fit or if you feel unwell from the cancer, these side-effects can be quite severe. Older patients in particular may benefit from less intensive types of chemotherapy.
Treatment of bone metastases: When bladder cancer has spread to the bone, skeletal complications can occur, such as weakening of the bones or pathological fractures from minor incidents or everyday activity. This causes pain and can have a detrimental effect on your quality of life. Your doctor may suggest radiotherapy, or drug treatment to help strengthen your bones and control the pain.
In addition, the recent experimental use of drugs called ‘immune checkpoint inhibitors’ in advanced bladder cancer appears effective in a subset of patients with this disease.
Q 13. What do do if my tumor comes back(=recurrence) after treatment?
A. Local recurrence: It takes place in the soft tissue where the bladder has been before removal or at the site of the lymph nodes that were removed. This is due to the fact that even after removal of the local pelvic lymph nodes, some nodes are left in place. Most local recurrences appear within the first 2 years. Local recurrence after complete removal of the urinary bladder is associated with poor overall prognosis but can occasionally be treated (surgery, chemotherapy, targeted radiation therapy).
Distant recurrence: If the cancer recurs outside the pelvis, it is a distant recurrence. This type of recurrence is fairly common after bladder removal in patients with high risk of recurrence (larger tumours, positive resection margins, involvement of the removed lymph nodes). Distant recurrence happens mostly within the first 2 years after bladder removal.
Sites of distant recurrences are lymph nodes, lungs, liver, and bones. Distant recurrence can be treated only by chemotherapy. Single or very few metastases may be surgically removed in addition to systemic treatment (= chemotherapy).
Recurrence in the urothelial tract (urethra and ureters): After complete removal of the bladder, the cancer can recur in the urethra, ureters and pelvis (urothelial tract). Most recurrences of the urothelial tract happen within the first 3 years after the operation. This type of recurrence is relatively rare.
If possible, a local treatment should be chosen to eliminate the cancer, unless systemic disease is suspected. In that case, chemotherapy or palliation should be used. In case of bladder preserving therapy and a superficial (non–muscle-invasive) recurrence, washing the bladder with drugs to prevent the growth or spread of cancer cells (instillation therapy) is advised.
Risk factors for recurrence in the urethra after removal of the bladder:
- Prior superficial (non–muscle-invasive) bladder cancer
- Multiple bladder tumours
- Tumour involvement of the bladder neck (and/or the prostate in men)
- An unused/residual urethra after incontinent urinary diversion
- Local recurrence in the lower pelvis
Although routine removal of the urethra (urethrectomy) is considered overtreatment, monitoring of the urethra is indicated in men.
Risk factors for recurrence in the ureters after removal of the bladder:
- Prior superficial (non–muscle-invasive) bladder cancer
- Multiple bladder tumours
- Tumour involvement at the opening (orifice) of the ureter
- Local recurrence in the pelvis
For patients with risk factors for urothelial recurrences, stringent or adapted monitoring is indicated.
Q 14. What is the Follow-up protocol?
A. After any kind of cancer treatment follow-up is essential to minimise complications and to detect and treat recurrences early. Follow-up protocol depends upon the stage of the disease and the treatment offered. These will be discussed in detail with you at the time of consultation.
Q 15. What are the symptoms of complications?
A. Functional complications after bladder removal include vitamin B12 deficiency, high acid levels in the blood (metabolic acidosis), worsening kidney function, urinary infections, urinary stone formation, tightening of stoma openings (stricture), other stoma complications in patients with ileal conduit diversions (leakage, inversion, skin irritation), neobladder continence problems, and emptying dysfunction.
unctional complications after bladder removal include vitamin B12 deficiency, high acid levels in the blood (metabolic acidosis), worsening kidney function, urinary infections, urinary stone formation, tightening of stoma openings (stricture), other stoma complications in patients with ileal conduit diversions (leakage, inversion, skin irritation), neobladder continence problems, and emptying dysfunction.
