Q 1. What is pelvic girdle pain (PGP)?
A. The pelvic girdle is a ring of bones around your body at the base of your spine. PGP is pain in the front and/or the back of your pelvis that can also affect other areas such as the hips or thighs. It can affect the sacroiliac joints at the back and/or the symphysis pubis joint at the front. PGP used to be known as symphysis pubis dysfunction (SPD).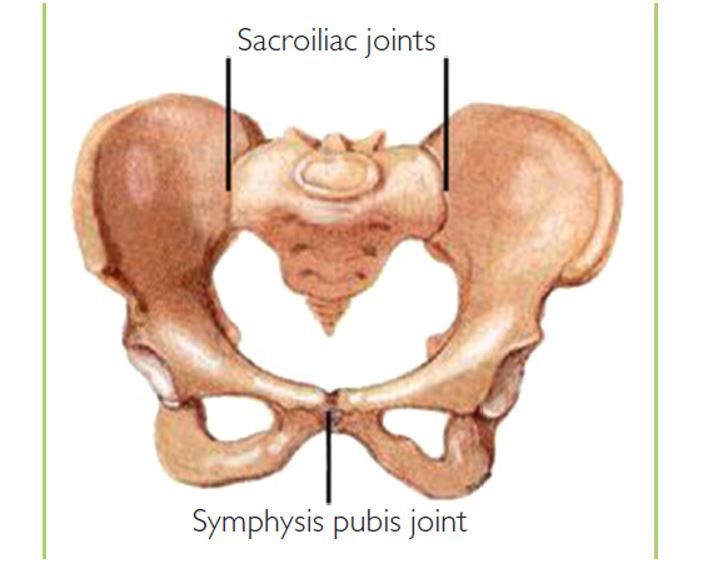
The pelvic girdle showing the sacroiliac joints and the symphysis pubis joint
PGP is common, affecting 1 in 5 pregnant women, and can affect your mobility and quality of life. Pain when you are walking, climbing stairs and turning over in bed are common symptoms of PGP. However, early diagnosis and treatment can relieve your pain. Treatment is safe at any stage during or after pregnancy.
Q 2. What causes PGP?
A. The three joints in the pelvis work together and normally move slightly. PGP is usually caused by the joints moving unevenly, which can lead to the pelvic girdle becoming less stable and therefore painful. As your baby grows in the womb, the extra weight and the change in the way you sit or stand will put more strain on your pelvis.
You are more likely to have PGP if you have had a back problem or have injured your pelvis in the past or have hypermobility syndrome, a condition in which your joints stretch more than normal.
Q 3. Can PGP harm my baby?
A. No.
Although PGP can be very painful for you, it will not harm your baby.
Q 4. What are the symptoms of PGP?
A. PGP can be mild to severe but is treatable at any stage in pregnancy and the sooner it is treated, the more likely you are to feel better. It is more common later in pregnancy.
Symptoms include:
- Pain in the pubic region, lower back, hips, groin, thighs or knees
- Clicking or grinding in the pelvic area
- Pain made worse by movement, for example:
- Walking on uneven surfaces/rough ground or for long distances
- Moving your knees apart, like getting in and out of the car
- Standing on one leg, like climbing the stairs, dressing or getting in or out of the bath
- Rolling over in bed
- During sexual intercourse.
Q 5. How is PGP diagnosed?
A. Tell your doctor about your pain.
You should be offered an appointment with a physiotherapist who will make an assessment to diagnose PGP.
This will involve looking at your posture and your back and hip movements and ruling out other causes of pelvic pain.
Q 6. What can I do to help my symptoms?
A. The following simple measures may help:
- Keeping active but also getting plenty of rest
- Standing tall with your bump and bottom tucked in a little
- Changing your position frequently – try not to sit for more than 30 minutes at a time
- Sitting to get dressed and undressed
- Putting equal weight on each leg when you stand
- Trying to keep your legs together when getting in and out of the car
- Lying on the less painful side while sleeping
- Keeping your knees together when turning over in bed
- Using a pillow under your bump and between your legs for extra support in bed.
You should avoid anything that may make your symptoms worse, such as:
- Lifting anything heavy, for example heavy shopping
- Going up and down the stairs too often
- Stooping, bending or twisting to lift or carry a toddler or baby on one hip
- Sitting on the floor, sitting twisted, or sitting or standing for long periods
- Standing on one leg or crossing your legs.
Q 7. What are my treatment options?
A. Your doctor will suggest the right treatment for you. This may include:
- Advice on avoiding movements that may be aggravating the pain. You will be given advice on the best positions for movement and rest and how to pace your activities to lessen your pain.
- Exercises that should help relieve your pain and allow you to move around more easily. They should also strengthen your abdominal and pelvic floor muscles to improve your balance and posture and make your spine more stable.
- Manual therapy (hands-on treatment) to the muscles and joints by a physiotherapist, osteopath or chiropractor who specialises in pgp in pregnancy. They will give you hands-on treatment to gently mobilise or move the joints to get them back into position, and help them move normally again. This should not be painful.
- Warm baths, or heat or ice packs
- Hydrotherapy
- Acupuncture
- A support belt or crutches.
For most women, early diagnosis and treatment should stop symptoms from getting worse, relieve your pain and help you continue with your normal everyday activities. It is therefore very important that you are referred for treatment early. PGP is not something you just have to ‘put up with’ until your baby is born.
Q 8. I’ve tried these measures but I’m still in pain. What are my options?
A. Being in severe pain and not being able to move around easily can be extremely distressing. Ask for help and support during your pregnancy and after the birth. Talk to your doctor if you feel you are struggling. If you continue to have severe pain or limited mobility, it is worth considering:
- Regular pain relief. Paracetamol is safe in pregnancy and may help if taken in regular doses. If you need stronger pain relief, your doctor will discuss this with you.
- Aids such as crutches or a wheelchair for you to use on a short-term basis. Your physiotherapist will be able to advise you about this. Equipment such as bath boards, shower chairs, bed levers and raised toilet seats may be available.
- Changes to your lifestyle such as getting help with regular household jobs or doing the shopping.
- If you work, talking to your employer about ways to help manage your pain. You shouldn’t be sitting for too long or lifting heavy weights. You may want to consider shortening your hours or stopping work earlier than you had planned if your symptoms are severe.
If you are in extreme pain or have very limited mobility, you may be offered admission to the antenatal ward where you will receive regular physiotherapy and pain relief. Being admitted to hospital every now and then may help you to manage your pain.
Q 9. Can I have a vaginal birth?
A. Yes.
Most women with pelvic pain in pregnancy can have a normal vaginal birth.
Make sure the team looking after you in labour know you have PGP. They will ensure your legs are supported, help you to change position and help you to move around.
All types of pain relief are possible, including an epidural.
Q 10. Do I need to have a caesarean section?
A. Caesarean section will not normally be needed for PGP. There is no evidence that a caesarean section helps women with PGP.
Q 11. Will I need to have labour started off (be induced) early?
A. Going into labour naturally is better for you and your baby.
Most women with PGP do not need to have labour started off.
Being induced carries risks to you and your baby, particularly if this is before your due date. Your midwife or obstetrician will talk to you about the risks and your options.
Q 12. What happens after the birth of my baby?
A. PGP usually improves after birth although around 1 in 10 women will have ongoing pain. If this is the case, it is important that you continue to receive treatment and take regular pain relief. If you have been given aids to help you get around, keep using them until the pain settles down.
If you have had severe PGP, you should take extra care when you move about.
Aim to become gradually more mobile. You should continue treatment and take painkillers until your symptoms are better.
If your pain persists, seek advice from your doctor, who may refer you to another specialist to exclude other causes such as hip problems or hypermobility syndrome.
Q 13. Will it happen in my next pregnancy?
A. If you have had PGP, you are more likely to have it in a future pregnancy. Making sure that you are as fit and healthy as possible before you get pregnant again may help or even prevent it recurring. Strengthening abdominal and pelvic floor muscles makes it less likely that you will get PGP in the next pregnancy.
If you get it again, treating it early should control or relieve your symptoms.
Q 14. Is there anything else I need to know?
A. Pregnant women have a higher risk of developing blood clots in the veins of their legs compared with women who are not pregnant. If you have very limited mobility, the risk of developing blood clots is increased. You will be advised to wear special stockings (graduated elastic compression stockings) and may need to have injections of heparin to reduce your risk of blood clots.
