Q 1. What is the umbilical cord?
A. The umbilical cord connects the baby from its umbilicus (tummy button) to the placenta inside the womb (uterus). The cord contains blood vessels that carry blood, rich in oxygen and nutrients, to the baby and take waste products away.
After the baby is born, the cord is clamped and cut before the placenta is delivered.
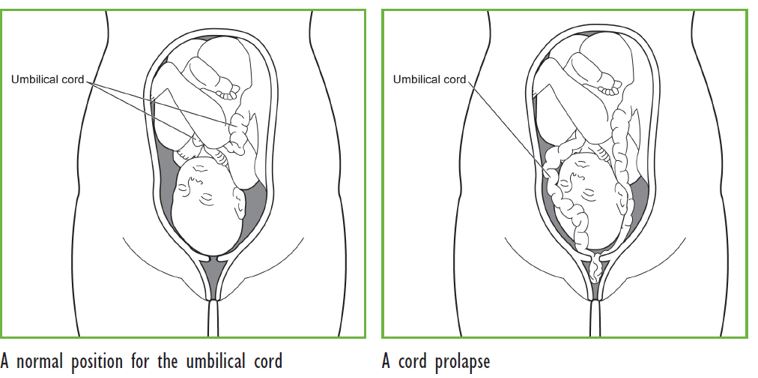
Q 2. What is an umbilical cord prolapse?
A. An umbilical cord prolapse happens when the umbilical cord slips down in front of baby after the waters have broken. The cord can then come through the open cervix (entrance of the womb). It usually happens during labour but can occur when the waters break before labour starts.
It is important to remember that:
- Cord prolapse is uncommon, occurring in between 1 in 200 and 1 in 1000 births
- When it does happen, it usually occurs close to the end of pregnancy (after 37 weeks)
- A prolapsed cord is an emergency situation for the baby.
Q 3. Why is it an emergency?
A. When the umbilical cord prolapses, it can be squeezed by the baby or the womb during a contraction. This can reduce the amount of blood flowing through the cord and so reduce the oxygen supply to the baby. The baby may need to be delivered immediately to prevent the lack of oxygen causing long-term harm or death of the baby.
Q 4. Can a cord prolapse be predicted?
A. It is not possible to predict a cord prolapse. An ultrasound scan does not show which women will have a cord prolapse, as the cord and the baby change position during the pregnancy.
Q 5. When is a cord prolapse more likely to happen?
A. When the baby is engaged (moves down into and completely fills the pelvis), the cord cannot usually prolapse. However, if the baby is not engaged, there is space for the cord to slip past and prolapse.
The chance of cord prolapse is higher if:
- Your baby is not in the head-first position, particularly if the baby is breech (bottom first) or transverse (lying sideways)
- Your waters break early or you go into labour prematurely
- You have more than one baby (such as twins or triplets)
- You have more water than usual surrounding your baby (polyhydramnios)
- You are having a small baby
- You have a low-lying placenta
- Your waters are broken by a doctor (artificial rupture of membranes or ARM) when the baby’s head is higher up in your pelvis. Your doctor will usually only break your waters if the baby’s head is low down in your pelvis to try to avoid cord prolapse. If there is uncertainty, your doctor might break the waters in an operating theatre. If there is a cord prolapse, you would then be in the best place to have your baby quickly.
Q 6. Can a cord prolapse be prevented?
A. Umbilical cord prolapse cannot be prevented. However, if you are at increased risk, you may be advised to be admitted to hospital – then immediate action can be taken if your waters break or you go into labour.
Your doctor will discuss with you the option of being admitted to hospital from 37 weeks if your baby is lying in a transverse position or is changing position frequently (unstable lie). This is because you are more likely to go into labour after this time.
Q 7. What are the signs of a cord prolapse?
A. The signs of a cord prolapse are:
- You can feel something (the cord) in your vagina
- You can see the cord coming from your vagina
- Your obstetrician can see or feel the cord in your vagina
- The baby’s heart rate slows (bradycardia) soon after your waters break. This can mean that the baby’s cord has been squeezed and the baby is not getting enough oxygen.
In some women there are no signs.
Q 8. What should I do if I am at home or at work?
A. If you think you can feel the cord in your vagina or you can see the cord, contact your obstetrician or hospital immediately and inform that you think you have a prolapsed umbilical cord.
- Do not attempt to push the cord back into your vagina
- Do not eat or drink anything in case you need an operation.
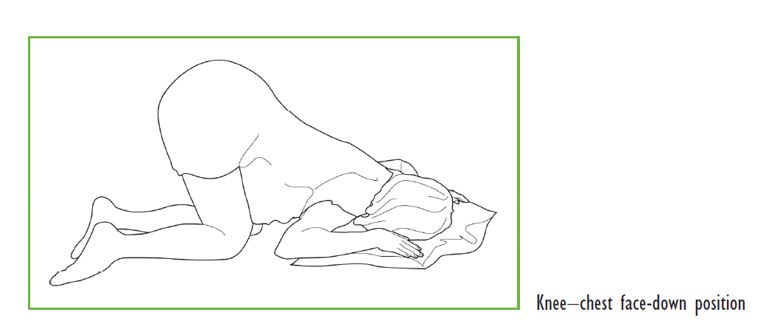
To reduce the risk of the cord becoming compressed, you will be advised to get onto your knees with your elbows and hands on the floor, and then bend forward.
You should remain in this position until the ambulance arrives.
The ambulance will take you to the hospital.
In the ambulance it is safer for you to lie down on your side.
Q 9. What happens next?
A. As your baby needs to be born as soon as possible, it is likely that you will be advised to have an emergency caesarean section but a vaginal birth may also be possible. Your doctor will explain the situation and what needs to be done.
The doctor may gently insert a hand in your vagina to lift the baby’s head to stop it squeezing the cord.
Sometimes a tube (catheter) may be put into your bladder to fill it up with fluid. This will help to hold the baby’s head away from the cord and reduce pressure on the cord.
You may be given oxygen through a mask and fluid from a drip.
Emergency caesarean section
If a vaginal birth is not possible quickly, you will be advised to have an emergency caesarean section.
You may need to have a general anaesthetic instead of a spinal or epidural anaesthetic for your caesarean section, so that the baby can be born quickly.
Vaginal birth
If your cervix is fully dilated, you may be able to have a normal birth or an assisted birth (forceps or ventouse) but only if this can happen quickly. A vaginal birth is less likely than a caesarean delivery when you have a cord prolapse.
Q 10. What could a cord prolapse mean for my baby?
A. For most babies, there is no long-term harm from cord prolapse.
However, even with the best care, some babies can suffer brain damage if there is a severe lack of oxygen (birth asphyxia).
Rarely, a baby can die.
Q 11. How will I feel after the birth?
A. For most babies, the outcome is good. However, the experience can be frightening for you, your partner and your family.
It is important to remember that the chance of having a cord prolapse in your next pregnancy remains very low.
